ARPwave Resources
Can Dual Wave Direct Current Electrical Stimulation Improve Motor Function in Chronic Stroke? – Results of a Longitudinal Case Study

Nick J. Siekirk1, Lisa Niles-Meunier2, Nisha Patel1, Jacob Bannister1, Robin Rosser1
1Motor Control Lab, Department of Health Sciences and Kinesiology, Georgia Southern University (Statesboro, GA, USA)
2Sports Therapy and Rehabilitation (Savannah, Georgia, USA)
Disclosure 1: The intervention was not reviewed by a local ethics committee and, as such, was not conducted with the approval of Georgia Southern University’s Institutional Review Board (IRB). The participant (identifiable only by initials; R.S.) was evaluated for contraindications and informed of the potential risks before providing written and verbal consent to participate.
Disclosure 2: ARPwave Technologies provided the modalities (RxBlack and FlexDoctor) on loan but did not influence the intervention’s methods or findings, nor was Nick J. Siekirk provided compensation (direct or indirect). ARPwave Technologies also did not define, influence, or restrict the scientific dissemination of findings (e.g., scientific presentation or publication).
Disclosure 3: The intervention was conducted as part of community outreach and was supervised by Lisa Bernadette Niles-Meunier, a licensed physical therapist (Georgia License Number PT002542).
Disclosure 4: Findings from this case study are descriptive and cannot be interpreted as causal. Descriptive improvements must consider thresholds for clinically meaningful changes.
SUMMARY
After seven weeks of pilot testing, a 74-year-old physically active (~6,000 to 8,000 steps per day) male participant (RS) (10 years and 5 months post left PCA and right basilar artery stroke) with spastic flexor tone underwent 12 total weeks of dwDC-NMES protocols.
- Gait changes were predominated by increased cadence (i.e., the number of steps per known distance), not spatial outcomes.
- Reduced timed up-and-go (TUG) time and increased 6-minute walk test (6MWT) distance improved mobility and gait capacity.
- Improved limits of stability (LOS) and static weight distribution indicate improved postural control. However, improvements in the center of pressure (COP) path length were not maintained in the interventions’ latter half.
- Relative to baseline, active extension of the affected wrist improved during weeks 5 – 10, but improvements were not maintained during week 12. Improvements in elbow extension were maintained with wrist pronation. Active dorsiflexion of the hemiparetic ankle increased.
- Subjective, self-reported depression (PHQ-9) and anxiety (GAD-7) symptoms were improved despite a worse perception of sleep quality (PSQI total score).
- Participant reported improvements in 5 of 7 sections of the Stroke Impact Scale.
BACKGROUND
Chronic Stroke
A stroke is an acute neurological event that disrupts the supply of blood and oxygen to the brain and can lead to temporary oxygen deprivation (e.g., a transient ischemic attack) or, in more severe cases, the death of brain cells (approximately 2 million per stroke minute) due to sustained blockage (i.e., ischemic stroke) or loss of vascular integrity (i.e., hemorrhagic stroke. Disability post-stroke is related to the stroke’s location, severity, and timeline between symptom onset and acute medical interventions. Notably, Georgia is among the “Stroke Belt,” a phrase coined to describe the 30% increase in stroke death rates observed in the Southeastern United States. Across the state, age-adjusted death rates are 10.8% – 11.4% higher than the national average, but, most notably, Georgia’s coastal plain (including Bulloch County) has a death rate 40% higher than the rest of the nation. Rural communities are plagued by commonplace lifestyle factors that increase the risk for chronic disease, and the increased death rates in the southeast are attributed to demographic and socioeconomic factors that are partly modifiable. Medical advances have improved the acute treatment of stroke, but improved survivorship means that more people are living with the residual physical and cognitive effects of stroke. Individuals returning to rural communities following a stroke require but often do not have access to ongoing therapies.
Problem Statement
Stroke is the leading cause of severe and long-term adult disability. Physical activity and structured exercise recommendations can mitigate these constraints by facilitating improvements in physical (e.g., mobility, physical activity levels) and psychological outcomes (e.g., anxiety/depression, perceived independence, and quality of life). However, low motivation, health concerns, ongoing fear of further or recurrent injury, and the lack of access to stroke-specific programs are prominent barriers to physical activity. Even with formal rehabilitation, exercise recommendations at discharge are vague and fixed with the expectation that they will be completed without supervision or social support. Exercise recommendations must be specific, goal-orientated, and structured to align and evolve (e.g., progress, regress) with the survivor’s needs to elicit continued improvement. To complicate matters, survivors must combat a stigma that advancing time does not allow further enhancements to unfold. Although relative improvement rates may wane with the advancement of time, exercise-induced improvements in aerobic capacity and gait function are possible in the chronic (>6 – months post-stroke) phase of recovery.
Direct Current Neuromuscular Stimulation
Direct current neuromuscular electrical stimulation (DC-NMES) uses external pads to administer high-frequency electrical impulses through the skin to nerves to assist homogenous muscle contractions and heighten sensory impulses. The use of DC-NMES in chronic stroke offers unique advantages. First, DC-NMES allows concurrent movement and can be used as an exercise adjunct. Intense exercise can release myokines (e.g., lactate, irisin, interleukin-6), a diverse group of peptides and proteins that stimulate neuronal growth, promote neuroprotective processes, and modulate inflammation. DC-NMES may attenuate neuronal inflammation and independently stimulate the expression of neurotrophic factors (e.g., brain-derived neurotrophic factor; BDNF) that attenuate stroke-associated neuronal loss by upregulating cascading processes that support neuronal growth, survival, and differentiation. Therefore, interventions combining exercise with dual wave DC-NMES could improve the exercise response and better mitigate residual motor impairments in chronic stroke.
Case Study Aim
The project aims to evaluate the longitudinal effect of dual-wave direct current neuromuscular electrical stimulation (dwDC-NMES) on motor function (e.g., mobility, postural control, fall risk) in chronic stroke (i.e., 6 months post-stroke).
Case Study Purposes
i. The primary purpose was to describe changes in gait, mobility, postural control, and active range of motion (ROM) while monitoring outside physical activity and sleep.
ii. The secondary purpose was to describe how dwDC-NMES affected resting blood pressure, heart rate, and post-exercise cardiovascular response.
iii. The tertiary purpose was to explore how DCES influenced subjective perceptions of stroke recovery, pain, and anxiety.
METHODS
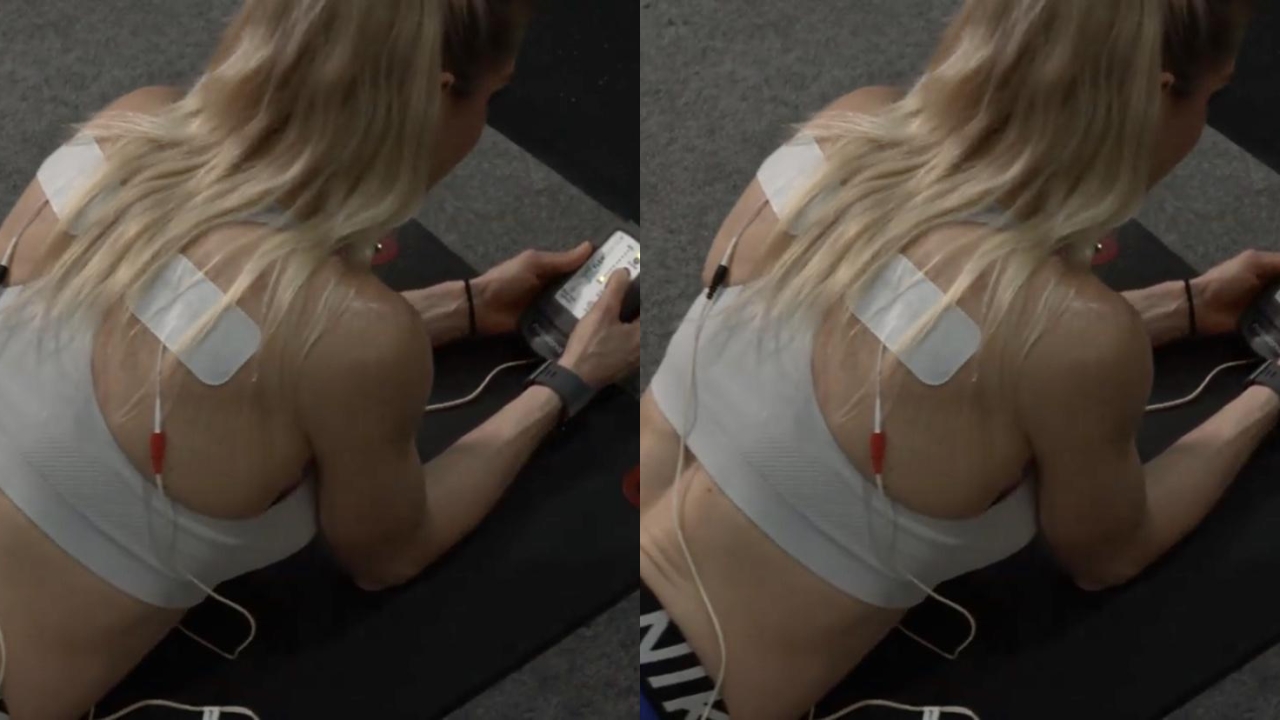
The U.S. Food and Drug Administration has approved dual-wave DC-NMES (RxBlack; ARPwave Technologies, Minneapolis, MN) as a Class II medical device.
RxBlack: After seven weeks of pilot testing, the 74-year-old male participant (RS) (10 years and 5 months post left PCA and right basilar artery stroke) underwent 12 total weeks of dwDC-NMES protocols in-lab at 432 – 999 pulses per second (pps) 1x/week (RxBlack, ARPWave, Minneapolis, MN). The 12-week RxBlack intervention consisted of three phases:
Phase 1: Three weeks of NeuroPattern Reset that focused on the affected upper extremity (UE)
Phase 2: Three weeks of NeuroPattern Reset that focused on the affected lower extremity (LE)
Phase 3: Five weeks of NeuroPattern Reset with a whole/full body (FB) focus.
FlexDoctor: In-lab dwDC-NMES protocols were supplemented with (n = 15 weeks) of concurrent at-home protocols: 1—the same exercise-focused warm-up protocol (termed NeuroEfficiency) performed in-lab (2x/day; 3 sets x 5 reps) and 2 – a passive recovery protocol (termed NeuroRecovery) (1x/day; 20 – 40 minutes) at 245 pps (FlexDoctor; ARPWave, Minneapolis, MN). The in-lab and at-home protocols are summarized in Table 1.

Measured Outcomes
Clinical and field-based (Timed Up and Go [TUG]; 6-Minute Walk Test [6MWT]) gait outcomes, bipedal postural control, and paretic range of motion measurements were completed before (Week 0), during (Week 8) and after (Week 14) the 12-week dwDC-NMES intervention (Tables 1 and 2). Active range of motions (aROM) are reported as joint excursions and were measured with a commercially available handheld dynamometer (Easy Angle, Meloqdevices, Stockholm, Sweden). Postural control outcomes included static weight distribution (WD), limits of stability (LOS), and balance/fall risk measurements using protocols provided by the manufacturer (Balance Tracker, San Diego, CA). Physical activity (steps/day) was monitored with a commercially available wrist wearable (Garmin International, Olathe, KS). Table 2 summarizes the timeline of measurements.
Table 1: Summary of dw-DC-NMES protocols.

Table 2: Timeline of Measured Outcomes.
†The American Geriatric Society and the British Geriatric Society guidelines recommend the Timed Up-and-Go Test (TUG) as a routine screening test for fall risk (Barry et al., 2014).
§The 6-minute walk test (6MWT) is associated with both treadmill and self-reported measures of functional performance while remaining sensitive to change with its ability to detect differences among different age and activity groups (Rikli & Jones, 1998).
›Strong correlations have been observed between the Stroke Impact Scale (SIS) 3.0 and the Barthel Index (BI) and the Instrumental Activities of Daily Life (IADL) scale (Vellone et al., 2015).
*The Pittsburgh Sleep Quality Index (PSQI) gained widespread acceptance as a valuable tool to measure sleep quality in different patient groups, such as those with sleep disorders, somatic diseases, or those living in nursing homes (Backhaus et al., 2002).
◦The strong association between Patient Health Questionnaire (PHQ-9) scores and functional status, disability days, and symptom-related difficulty established construct validity (Kroenke et al., 2001).
•The association between Generalized Anxiety Disorder (GAD-7) with measures such as depression, self-esteem, life satisfaction, resilience, and the demographic risk factors of generalized anxiety disorder suggests the construct validity of GAD-7 in the general population (Löwe et al., 2008).
RESULTS
i. The primary purpose was to describe changes in a gait, b mobility, c postural control, and d active range of motion (ROM) while monitoring outside physical activity and sleep.
Clinical Gait Outcomes (GaitRITE)
• Forward-fast gait velocity improved +0.02 m/sec from 1.80 m/sec to 1.82 m/sec by increased cadence (+16 steps/cycle) and not symmetrical step/stride length or swing/stance improvements between the Aleg and NaLeg.
• Cadence (i.e., the measure of how many steps or cycles a person takes per known distance) increased by 16 steps/cycle from 145 to 161 steps/cycle.

• Step length was reduced by 4.0 cm on the affected leg (Aleg) and 8.6 cm on the non-affected leg (NaLeg)
• Stride length was reduced by 16.0 cm on the Aleg and 12.10 cm NaLeg.

• Step length on the Aleg was greater than NaLeg at all time points. Step length asymmetry was calculated (Aleg – NaLeg) and ranged from 6.50 cm (9/13/24) to 25.15 cm (11.6.24). Step length asymmetry (post – pre) increased by 4.55 cm from 8.16 cm (Aleg > NaLeg) to 12.71 cm (Aleg > NaLeg).
• Stride length on the NaLeg was greater than the Aleg at 5 of 8 time points. Stride length asymmetry was calculated (Aleg – NaLeg) and ranged from -4.07 cm (13/13/24) to 4.24 cm (9.13.24). Step length asymmetry (post – pre) decreased by 3.55 cm from -0.19 cm (NaLeg > Aleg) to -4.07 cm (NaLeg > Aleg).

• Swing time on the Aleg was greater than the NaLeg at all time points. Swing time was reduced by 0.04 seconds (sec) on the Aleg and 0.03 sec on the NaLeg.
• Stance time on the Aleg was less than the NaLeg at all time points. Stance time was reduced by 0.07 seconds (sec) on the Aleg and 0.06 sec on the NaLeg.

Mobility: Timed Up and Go (TUG) and Gait Capacity/Endurance: 6 Minute Walk Test (6MWT)
• Improvements in TUG time (Δ = -0.26 sec) and 6MWT (Δ = +87 m) distance were observed between pre-intervention Assessment 1 (8/9/24) and Assessment 3 (11/13/24).
Postural Control Outcomes (Balance Tracker)
• Limits of stability (LOS):
i. Post-treatment results showed increased area for three metrics
1. Back Left: +19 cm2
2. Back Right: +163 cm2
3. Total Area: +170 cm2
ii. The LOS area did not change for the forward right.
iii. The LOS area for the forward left was reduced by 12 cm2
• Weight Distribution (WD):
i. The left (affected)/right (non-affected) weight distribution post-treatment improved (Pre = 45/55; Post = 48/52), closer to the ideal 50/50 distribution.
ii. Post-treatment, The front/back weight distribution improved (Pre = 66/34; Post = 61/35).
• Balance and Fall Risk (B&FR)
i. Center of Pressure (COP) path length improved 15% from 30cm (72nd percentile) pre-intervention (Assessment 1) to 26cm at Assessment 2 (87th percentile). R.S. was considered low risk for falls at Assessments 1 and 2.
ii. COP path length regressed 13% from 26 cm at Assessment 2 (72nd percentile) to 34 cm at Assessment 3 (67th percentile). Based on Assessment 3 results,
Active Range of Motion (aROM) – Ankle Dorsiflexion
Note: From terminal plantarflexion (20◦ to 30◦ from neutral), expected dorsiflexion ROM is 40◦ to 70◦.
• Active ankle dorsiflexion improved 20◦ from 16◦ (8/28/24) to 33◦ (11/13/24), a 106% improvement (25% clinical meaningful threshold) or 81% above the approximate threshold. i. All measurements after (8/28/24) were improved and sustained (see the red dashed line on the graph below).
ii. Absolute daily improvements (ΔDF: calculated as post – pre) ranged from -2◦ to +8◦ (8/28/24 to 9/25/24).
• Results suggest the ankle was susceptible to early dorsiflexion improvements, but improvements were sustained.

Ankle Dorsiflexion Active Range of Motion (aROM): Active ankle excursion was measured from passive terminal plantarflexion to active terminal dorsiflexion. DF_PRE: Ankle excursion at arrival before DC-NMES. DF_PostTx: Ankle joint excursion after DC-NMES. ΔDF: Change in ankle excursion, calculated as (post-treatment – pre-treatment) on each measurement day.
Active Range of Motion (aROM) – Wrist Extension
Note: Expected extension range of motion at the wrist is ~70◦ from neutral.
• Active wrist extension improved 18◦ from 54◦ (8/28/24) to 72◦ (10/16/24), a 33% improvement.
i. Measurements after (8/28/24) were improved and sustained until (10/16/24) (see the red dashed line on the graph below).
• Wrist extension reduced 25◦ (-37%) between (10/16/24) and (11/13/24) suggesting that previous measurements were inflated (e.g., assisted by elbow flexion), R.S. experienced increased spasticity or a loss of aROM due to non-specific training.

Wrist Extension Active Range of Motion (aROM): Active wrist excursion was measured supine with the wrist neural and palm supinated, the shoulder abducted to 30 – 40◦. WristExt_PRE: Wrist excursion at arrival before DC-NMES. WristExt_PostTx: Wrist excursion after DC-NMES. ΔWristExt: Change in wrist excursion, calculated as (post-treatment – pre-treatment) on each measurement day.
Active Range of Motion (aROM) – Elbow Extension with Wrist Supinated
• Active elbow extension improved 25◦ from 102◦ (8/28/24) to 127◦ (11/13/24), an approximate 25% improvement.
i. Measurements after (8/28/24) were improved and sustained until (10/23/24) (see the red dashed line on the graph below).
• Elbow extension reduced 16◦ (-14%) between (10/23/24) and (11/13/24) suggesting that R.S. experienced increased spasticity or a loss of aROM due to non-specific training.

Elbow Extension Active Range of Motion (aROM): Active elbow excursion was measured from passive terminal flexion with the palm supinated, the shoulder abducted to 30 – 40◦. ElbowExt_Supinated_PRE: Elbow excursion at arrival before DC-NMES. ElbowExt_Supinated_PostTx: Elbow excursion after DC-NMES. ΔElbowExt_Supinated: Change in elbow excursion, calculated as (post-treatment – pre-treatment) on each measurement day.
Active Range of Motion (aROM) – Elbow Extension with Wrist Pronated
• Active elbow extension improved 11◦ from 131◦ (8/28/24) to 142◦ (11/13/24), an 8% improvement.
i. All pre-treatment measurements after (8/28/24) were improved or sustained over the 12-week intervention (see the red dashed line below).

Elbow Extension Active Range of Motion (aROM): Active elbow excursion was measured from passive terminal flexion with the palm supinated, the shoulder abducted to 30 – 40◦. ElbowExt_Supinated_PRE: Elbow excursion at arrival before DC-NMES. ElbowExt_Supinated_PostTx: Elbow excursion after DC-NMES. ΔElbowExt_Supinated: Change in elbow excursion, calculated as (post-treatment – pre-treatment) on each measurement day.
ii. The second purpose was to describe how DCES affected resting and post-exercise blood pressure and heart rates.
• Post-Exercise BP
i. SBP recovery improved by 4 mmHg in the second and third minutes compared to baseline (8/9/24) at Week 8 (10/2/24).
ii. Peak SBP and DBP were greater after 6MWT on (11/13/24) than Assessment 2 (10/2/24) and Assessment 1 (8/9/24). This may be attributed to an increased SBP upon arrival. Nevertheless, HR and DBP returned to resting levels within 5 minutes of passive rest.
• Post-Exercise HR
i. HRpeak post 6MWT was reduced post-treatment on (10/2/24) by 6 bpm despite the increased walking distance.
ii. Unlike baseline, HR recovered to pre-exercise measurement in the second minute of rest post-6MWT (10/2/24).
iii. Increased HR post 6MWT during the 4th recovery minute is attributed to an automated cuff error (11/13/24).
iii. The third purpose was to explore how DCES influenced subjective perceptions of sleep, stroke recovery, and depression/anxiety.
• Depression (PHQ-9)
i. PHQ-9 total score was reduced by five after the 12-week intervention.
• Anxiety (GAD-7)
i. GAD-7 total score was reduced by four after the 12-week intervention.
• Sleep (Pittsburg Sleep Questionnaire)
i. Global Score 1. PSQI global score increased from 5 (pre-treatment) to 7 (post-treatment).
• Stroke Recovery (Stroke Impact Scale)
i. Strength
1. No change in perceived strength from Assessment 1 to Assessment 3.
2. Improved perception of strength from Assessment 2 to Assessment 3.
ii. Memory and Thinking
1. No change in perceived memory and thinking.
iii. Mood and Emotional Control
1. Median improvement of +1 over the 12-week intervention from Assessment 1 to Assessment 3.
iv. Communication
1. No change in perceived ability to communicate.
v. Activities of Daily Living
1. Median improvement of +0.5 (i.e., reduced perceived difficulty) over the 12-week intervention.
vi. Mobility
1. Median improvement of +1 over the 12-week intervention from “a little difficult” to “not difficult at all.”
vii. Hand Function
1. No change in perceived hand function.
viii. Participation in Roles
1. Median improvement of +1 over the 12-week intervention from Assessment 1 to Assessment 3.
2. Median improvement of +2 from Assessment 2 to Assessment 3.
References
Barry, E., Galvin, R., Keogh, C., Horgan, F., & Fahey, T. (2014). Is the Timed Up and Go test a useful predictor of risk of falls in community dwelling older adults: asystematic review and meta-analysis. BMC geriatrics, 14, 1-14.
Rikli, R. E., & Jones, C. J. (1998). The reliability and validity of a 6-minute walk test asa measure of physical endurance in older adults. Journal of aging and physical activity, 6(4), 363-375.
Vellone, E., Savini, S., Fida, R., Dickson, V. V., Melkus, G. D. E., Carod-Artal, F. J. & Alvaro, R. (2015). Psychometric evaluation of the stroke impact scale 3.0. Journal of Cardiovascular Nursing, 30(3), 229-241.
Backhaus, J., Junghanns, K., Broocks, A., Riemann, D., & Hohagen, F. (2002). Test retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. Journal of psychosomatic research, 53(3), 737-740.
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ‐9: validity of a brief depression severity measure. Journal of general internal medicine, 16(9), 606-613.
Löwe, B., Decker, O., Müller, S., Brähler, E., Schellberg, D., Herzog, W., & Herzberg, P.Y. (2008). Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Medical care, 46(3), 266-274.